Addison’s Disease and Adrenal Insufficiency
What is Addison’s Disease? What are the symptoms?
Addison’s disease, or primary adrenal insufficiency, develops when your adrenal glands do not produce enough of the hormone called cortisol. This can be due to a problem within the adrenals (primary adrenal insufficiency) or due to a problem within the pituitary gland, a part of the brain which produces the hormone (ACTH) that sends instructions to the adrenals to make cortisol. When the pituitary is damaged the loss of ACTH can be the cause of adrenal cortisol deficiency (secondary adrenal insufficiency).
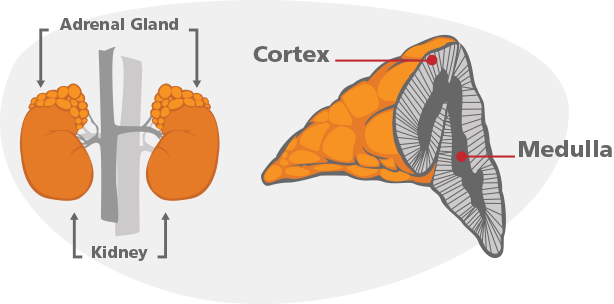
People with primary adrenal insufficiency (Addison’s disease) usually don’t make enough of an additional hormone called aldosterone; so in addition to taking cortisol replacement, they also need aldosterone replacement. People with secondary adrenal insufficiency are only low on cortisol and do not need aldosterone replacement. Cortisol and aldosterone are just two of the more than 50 hormones the adrenal glands generate. The adrenal glands sit directly above each kidney.
Symptoms of primary or secondary adrenal insufficiency may slowly develop and progress. Common symptoms include:
• Weakness
• Fatigue
• Abdominal pain
• Nausea
• Weight loss
• Low blood pressure
• Darkened skin (in the case of Addison’s disease)
• Salt craving (in the case of Addison’s disease)
• Dizziness upon standing
• Depression
• Lab tests may show low sodium and/or high potassium levels
Addison’s Disease Causes
Primary Adrenal Insufficiency: Addison’s Disease
The outer layer of the adrenal glands is called the adrenal cortex, which makes the hormone cortisol.
The most common cause of primary adrenal insufficiency in the United States is an autoimmune disease that causes the immune system to destroy the adrenals with an antibody. Other reasons that adrenal glands are destroyed can be tuberculosis, bleeding into the adrenal glands, cancers or other rare infections.
Polyendocrine autoimmune syndrome is a rare combination where multiple endocrine organs are destroyed by the immune system, which can include Addison’s disease. Sometimes referred to as multiple endocrine deficiency syndrome and develop in adults aged 18-30.
Associated conditions include:
• Addison’s disease
• Underactive or overactive thyroid function (Hypothyroidism or Hyperthyroidism)
• Delayed or slow sexual development (Hypogonadism)
• Diabetes (Insulin deficiency)
• White skin patches (Vitiligo)
• Celiac disease
When people with polyendocrine autoimmune syndrome are affected by Addison’s disease and thyroid disease, it is called Schmidt’s syndrome.
Secondary Adrenal Insufficiency: ACTH Deficiency
Secondary adrenal insufficiency is caused by damage to the pituitary gland which makes the hormone called adrenocorticotropic hormone (ACTH). It is your brain’s signal to the adrenal glands, telling them to make cortisol.
By far the most common cause of this type of adrenal insufficiency is due to chronic oral steroid medications. When steroids (which have the same action as cortisol) are taken to treat other medical conditions the brain stops sending the signal of ACTH to the adrenal glands to make the body’s own cortisol. Once steroids are stopped, it can take a long time for the brain to resume making ACTH, so the adrenals may take a long time to “wake up” and for the adrenal to start working again.
ACTH production is decreased by several other conditions and therefore hinders cortisol secretion:
• Loss of blood flow (circulation) to the pituitary gland or bleeding into the pituitary
• Pituitary tumor, or other brain tumors that puts pressure on the pituitary
• Radiation treatment of the pituitary
• Surgery near the pituitary gland or hypothalamus
• Severe head injury
• Severe infection
Diagnosis of Adrenal Insufficiency
In trying to diagnose primary or secondary adrenal insufficiency, your endocrinologist typically needs a physical exam and laboratory tests before treatment. This will help the doctor narrow down your condition to make the correct diagnosis because your symptoms may be confused with other disorders.
A physical examination that includes a thorough review of your medical and family history, laboratory tests and imaging tests of the adrenal and/or the pituitary are usually needed to confirm the diagnosis.
Baseline Laboratory Testing
The first step to detect abnormal adrenal function may be to measure your cortisol and ACTH levels. Cortisol levels follow a natural cycle throughout the day; they are highest in the morning, so most likely you doctor will want to draw these labs around 8 to 9 am. The “gold standard” test to diagnose adrenal insufficiency is the ACTH Stimulation Test. This is typically an intravenous test done in an infusion room and may be done anytime of the day. To begin the ACTH stimulation test, an IV line is placed and blood is drawn to measure the cortisol and ACTH level. Next, cosyntropin (a synthetic derivative of ACTH) is injected, and then after 30 minutes blood is drawn again to re-evaluate your adrenal’s response to stimulation. A normal response after cosyntropin injection is an increased cortisol level. An abnormal response is too little cortisol released. If the test is abnormal, a repeat ACTH is necessary to confirm the diagnosis.
Imaging Test: CT and MRI Scans
A CT scan of your adrenals and a MRI scan of your brain provide a picture of your adrenal and pituitary glands. The shape and size of each gland may be helpful to diagnose why there is diminished function of the adrenal gland. The MRI of the pituitary may be helpful to diagnose pituitary causes of secondary adrenal insufficiency.
The imaging tests listed above can support a diagnosis of adrenal insufficiency, but your doctor shouldn’t definitively diagnose the disorder from these imaging tests. The hormone tests are what make the diagnosis, but imaging tests can provide further supporting information as to the possible cause.
Adrenal Insufficiency Treatment
Cortisol is the corner stone of adrenal replacement therapy and is replaced with hydrocortisone, prednisone or other less frequently used forms of therapy. Aldosterone is replaced with an oral mineralocorticoid, called Florinef or fludrocortisone. Your doctor may also recommend you increase your salt intake, as well to help this medication to be most effective.
Your doctor will provide you with dosing instructions including how many pills to take each day, the best time to take the hormone, and common side effects. He or she will closely monitor your symptoms and lab tests to make sure your dose is sufficient, without giving you too much of the replacement hormone.
Important Medications Notes
• It is important to take your medication as directed by your doctor. If you vomit up your mediation or are too ill to take it, immediately contact your doctor or call 9-1-1.
• If you have been diagnosed with adrenal insufficiency, you should wear a medial identification bracelet or necklace at all times should an emergency develop. A wallet card may also be helpful.
• In emergency situations it may be necessary to get an emergency injection which should be discussed with your provider.
Adrenal Insufficiency: When It Becomes a Crisis
The symptoms of adrenal insufficiency may slowly develop and progress. Sometimes a stressful event, infection or illness causes Adrenal Crisis which is a condition that merits urgent medical attention because lack of enough cortisol can be fatal.
The symptoms of an adrenal crisis include:
• Dehydration and/or severe vomiting and diarrhea
• Stabbing pain in the abdomen, low back and legs
• Low blood pressure (shock)
• Low blood sugar
• Loss of consciousness
Life-saving treatment with steroids can only be given if the emergency medical team knows that you have adrenal insufficiency; the symptoms of adrenal crisis can affect your thinking and even cause loss of consciousness, so it’s essential that all patients with adrenal insufficiency wear a medical alert bracelet or necklace that clearly states their diagnosis.
Adrenal Crisis Management and Prevention
Adrenal crisis is an emergency, as it can be fatal. Treatment for adrenal crisis may include intramuscular or intravenous injection of glucocorticoid, salt water (saline), and sugar (dextrose). Adrenal crisis is best managed within an emergency room or intensive care unit. Do not delay in having someone take you to the hospital or call 9-1-1.
Your doctor will help you to identify signs, symptoms, and stressors that may trigger adrenal crisis. Always contact your doctor if you are worried that you might have an adrenal crisis. Sometimes, crisis can be averted with oral medication your doctor prescribes (i.e. prednisone or anti-nausea medicine). He or she will also teach you when and how to give yourself an emergency steroid injection.
Outlook
While adrenal insufficiency is a rare but serious disorder, most patients live normal, happy lives. Treatment is required life-long and is essential to keep you feeling healthy.
![]()